MSK: Healthy Bones and Bone Biology
Healthy Bones and Metabolism


High strain
Bones consists of: Mineral and Organic part
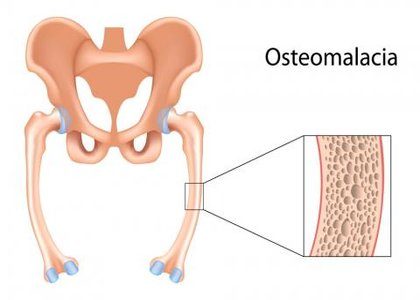
Calcium hydroxyapatite - provides compressive strength - lack of mineral components of bone results in rubbery and flexible bones = osteomalacia
- Collagen (tensile strength) (PG- compressive strength)
- Proteoglycans - provides flexible strength- lack of organic results in brittle bone disease
- Osteocalcin (promotes mineralisation)

Ca2+ is produced from:
- Bone turnover
- Resorption from kidneys
- Diet
The regulation of Ca2+ is by:
- PTH
- Vitamin D
- Calcitonin
The amount of Ca2+ is instrumental for the bone density - a measure of the mineral present in bone.
Bone density can be affected by a range of factors including:
- Availability of substrates - Ca2+ intake/absorption and PTH function
- Physiological - Weight bearing exercise/ Smoking/ Diet + BMI
- Biochemical - Hormones/ Steroid/ Menopause
Bone density varies with age and exercise. Hormones and exercise help with bone structure as they add to the mineral pool.
Actions of PTH
Formation of Vitamin D
To increase the formation of Vitamin D:
- Increased PTH
- Decreased PO4-
- Decreased 1,25 (OH) D
Action of Vitamin D
Bone Biology
Bone cells:
- Osteochondral progenitor cells - undifferentiated stem cells
- Osteoblast - lays down bone
- Osteoclasts - resorbs bone
- Osteocytes - mature bone in lacunae
- Bone lining - regulates movement of PO4- and Ca2+
Bone types:
- Long eg. femur
- Flat eg. scapula
- Short eg. carpal
- Irregular eg. C6
There are 2 types of bone - CORTICAL and TRABECULAR

Plates of bone arranged along lines of stress. Haversian canal with lamallae
Cavities are filled with matrix
Bones need to grow both in width and length. These occur in different ways.
Width: (appositional)
- Osteoblasts in the periosteum secrete matrix + are trapped as osteocytes
- Osteoclasts, increase the diameter of the medullary cavity
- Increased diameter until skeletal maturity
Length: (endochondral)
- Interstitial growth from cartilage
- Occurs at the epiphyseal growth plates
- Stops when the growth plates ossify
Bone remodelling is a dynamic process and is effected by Wolff's Law. This states that bone adapts to the mechanical environment.
Increased stress - increased osteoblast activity = more bone
Decreased stress - decreased osteoblast activity = less bone
Cartilage
Types of cartilage:
- Fibrocartilage - v. hard eg. knee - meniscus
- Hyaline- end of long bones + growth plates
- Elastic - tubular open structure
Growth occurs either by appositional or interstitial growth
Articular cartilage -found at the end of long bones.
Function:
- Smooth - decreases friction
- Deformable and elastic
- Distributes load evenly
- Increases SA therefore decreases force
- High stiffness
- Creep (deformation under loading)
Growth:
- Column of cells - bone matrix - calcified cartilage - bone
- Abundance of collagen at the surface
- Arcades of type II collagen fibrils anchor proteoglycan matrix to bone
Adult articular cartilage is:
- Hypocellular
- Aneural
- Avascular
Cartilage metabolism is affected by mechanical factors. Anabolic and catabolic processes are adjusted to adapt to matrix after mechanical demands.
Load > 1Mpa = Anabolic
Load < 1 Mpa = Catabolic
Also involves adaptive remodelling:
High strain
Leads to matrix deposition
Increased matrix stiffens
Low strain
Matrix resorption
Decreased matrix stiffnes
However cartilage injury proves to be difficult as:
- No capillaries
- Nutrients are gained from diffusion
- Chondrocytes don't divide in adults
Effect of aging on cartilage:
• Decreased PG & collagen turnover
- Collagen disruption
- PGs lost
- Water lost on compression
- Tissue damage
•Increased non-enzymatic glycation (NEG)
- makes bones more brittle and can't support load
• Impaired joint lubrication
- friction / heat
- fibrillation
- osteoarthritis







Comments
Post a Comment