MSK: Fractures and Muscle Pain
Bone Fractures and Healing











Covered by periosteum that helps with fracture healing. Contains osteogenic progenitor cells that mature into osteoblasts and therefore increases the thickness.
Two types of bone: CORTICAL and TRABECULAR
Cortical bones have a strong outer layer which resists force and weight. It is organised into Haversian systems.

Consists of concentric lamallae - rings of calcified matrix.
Contains osteoblasts embedded in lamallae which mature and become osteocytes in lacunae.
Canaliculi - connect lacunae and are used in the movement of nutrients and removal of waste products.
Osteoclasts

Has a ruffled border - attaches to the surface of bone and releases lysosomal enzymes and acids which act to digest the proteins found in the bone matrix. These are balanced with osteoblasts.
Osteopetrosis: OC can't create acidic conditions to absorb bone which results in dense bones.

Bone Remodelling
- Re-absorption: Osteoclasts attach themselves to the surface of the bone. Protein and Ca2+ are secreted into the extracellular space by OC
- Formation: Osteoblasts migrate to the hollowed out bone and form Type I collagen which are coated in Ca2+ = new bone
- Remodelling: woven bone lattice is rearranged into cortical and spongy bone lattice.
This woven bone is removed by osteoclasts.
Remodelling is affected by a range of factors, including:
- Mechanical
- Genes - potential size and shape/ GH release/ Hormone receptors on bone cells
- Hormones - Growth,sex and thyroid affect cell differentiation and metabolism
- Aging - OB decrease vs. OC, decreased collagen = brittle
- Disease - osteoporosis (cancellous bone is most affected)
Cutting Cone
Remodelling of cortical bone.

- Osteoclastic resorption
- Layering of OB
- Layering of lamallae
OC make the head and followed by capillaries and then OB that lay down osteoid
Stages of Fracture Healing
1. Haematoma

- Blood vessels cross into the fracture line and leak
- Blood clot forms
- Blood supply is disrupted on either side of the bone and dies
- Macrophages and OC move to the site and remove them = swelling
- Blood capillaries grow into the space
2. Soft Callous
- Blood vessels form granulation tissue = pro callous
- Fibroblasts and osteogenic progenitor cells invade the pro callous to form the bone matrix
- The callous which is formed is v.v. soft
3. Hard callous

- Osteogenic progenitor cells form osteoblasts and secrete matrix
- Forms trabeculae
- Trabeculae joins either side of the bone
Types of Non-Union
Hypertrophic Non Union
Callous has formed but the fracture has not joined. Can be due to inadequate fixation of fracture and can be fixed by rigid immobilisation.
Atrophic Non Union

No callus is formed. This is often due to impaired bony healing, for example due to vascular causes (e.g. impaired blood supply to the bone fragments) or metabolic causes (e.g. diabetes or smoking).
Atrophic non-union can be treated by improving fixation, removing the end layer of bone to provide raw ends for healing, and the use of bone grafts.
Muscle Pain During and After Exercise
Function:
SR Stores/releases/restores Ca2+
T Tubules Convey AP down membrane v. quickly
DHP Receptors Voltage sensors
Ryanodine Ca2+ release channels
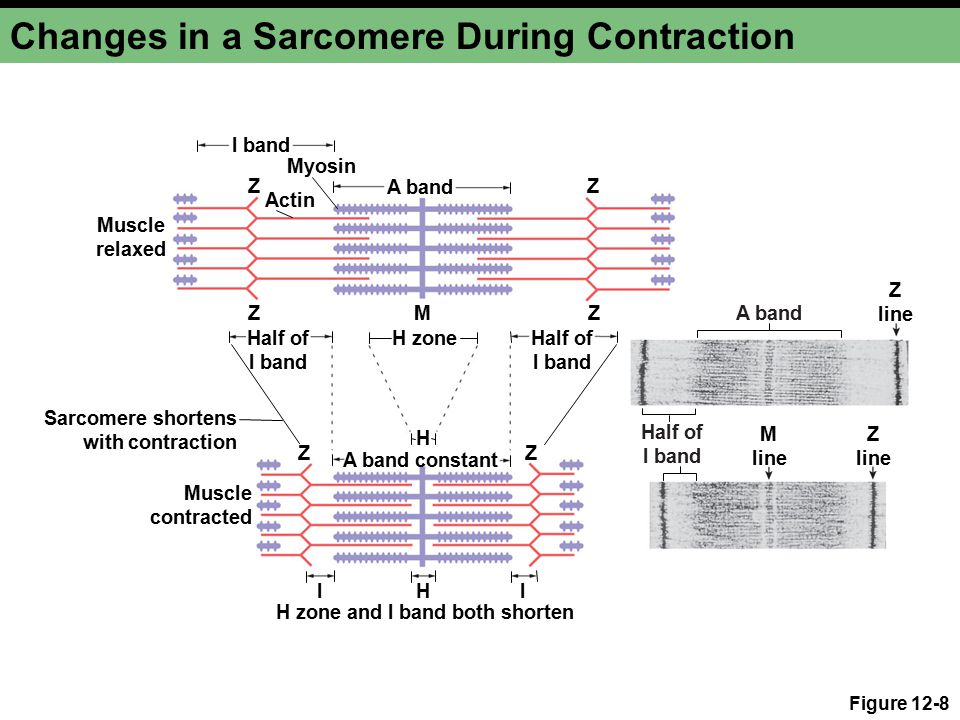
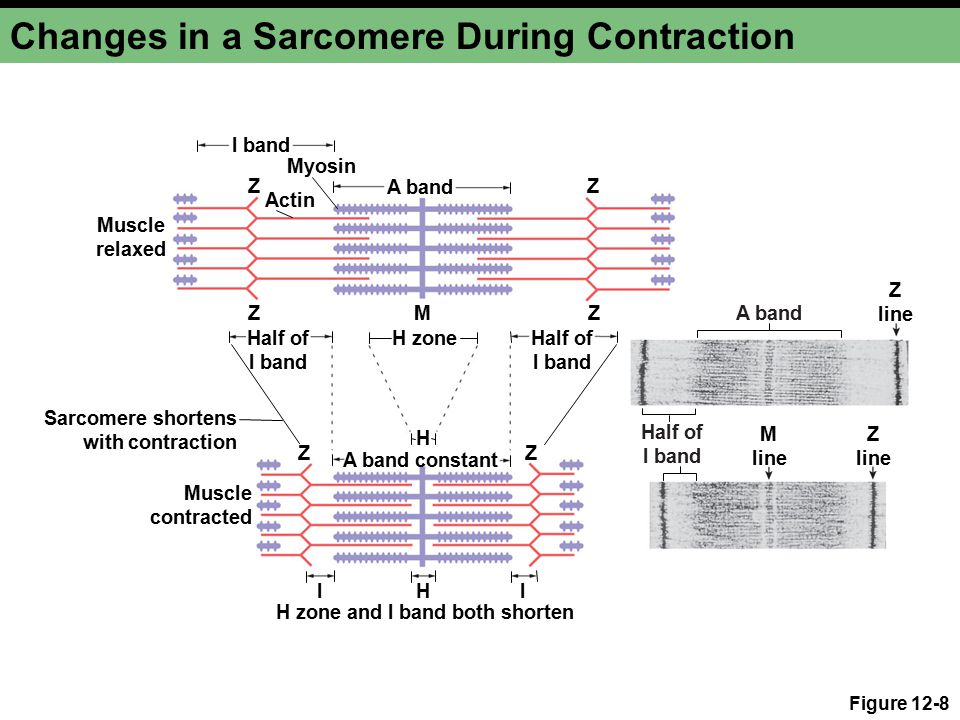
2 types of muscle contraction:
Isotonic - muscle changes length without change tension
Isometric - length doesn't change
Botulinum Toxin:

- Prevents release of ACh by damaging proteins
- Reduces the release of ACh
- Causes the paralysis of muscles and the loss in muscle tone
- Used to block muscle spasms in MS
Curare:
- Blocks binding of ACh to nACh receptors receptors therefore no muscle contraction
- Used to relax muscles during surgery
Suxamethionine:
- Opens nAChRs to cause long lasting depolarisation therefore synapse is blocked
- Used to relax laryngel muscles to facilitate intubation
- Can cause hyperkalemia as K+ channels to open
- Delayed muscle pain and bradycardia
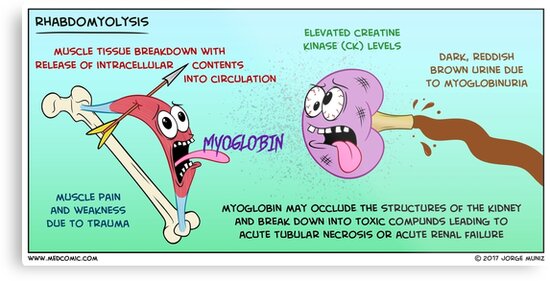
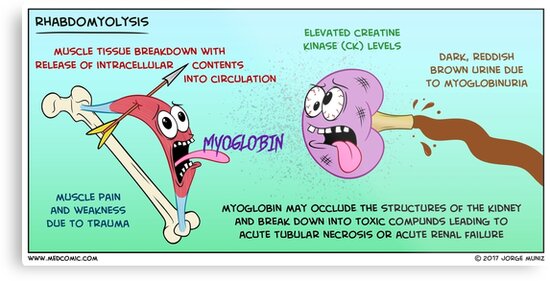
Rhabdomyolysis: damaged skeletal muscle breaks down and muscle content enters circulation. Myoglobin is found in the urine.
Tetanus Toxin - prevents functioning of inhibitory motor neurons
Mechanism of Action:
- Bound to presynaptic terminals of NMJ
- Transported to spinal cord by MN + transferred to inhibitory presynaptic terminals
- Destroys VAMP + inactivates inhibitory neurotransmission that suppresses MN and muscle activity
Results in hyper-excitability and lock jaw
Types of Skeletal Muscle
Slow - oxidative (I)
- small diameter
- high myoglobin
- lots of mitochondria
- high capillary density
- low GEC
Low Vmax - speed of contraction. Slow cross bridge cycling. Slow rate of shortening.
Fast - glycolytic
- large diameter
- low myoglobin
- few mitochondria
- low capillary density
- high GEC
High Vmax. Fast cross bridge cycling. Fast rate of shortening
Effect of Exercise on Muscles
Fatigue
Central (neural):
- Unable to maintain effort
- Reduced motor neurone activity
Peripheral (muscular):
- Decreased electrical stimulation of motor neurones
- Decreased Ca2+ release
- No transmission at NMJ
Pain after exercise:
- Inflammation
- Muscle damage
- Activation of sensory nerves by lactate, pH and ATP
Muscle damage after exercise:
- Delayed onset muscle soreness
- Changes post marathon - inflammatory cytokines which reduce power by 30%
- Dystrophin - support muscle fibre strength
Satellite Cells: Muscle stem cells that repair damage. A decrease = sarcopaenia


Comments
Post a Comment