Urinary: Glomerular Filtration and Tubular Reabsorption
Glomerular Filtration
180L (plasma) filtered but 175L reabsorbed. Governed by GFR.
GFR: the speed at which the filtrate passes across the 3 barriers. Usually 100ml/min which is fixed in healthy individuals.
3 barriers involved in filtration:
- Fenestrations - filters by size
- Basement membrane- filters by charge as it's -vely charged (MAIN BARRIER)
- Podocytes - 3rd back up component
- No cells
- Trace amount of proteins
- Ions and small organic substances in the same conc. as plasma
The rate of filtration depends on:
- Molecular weight - inversely proportional
- Charge - positively charged >> neutral >> negatively charged
- Shape - long, thin molecules are filtered more easily than spherical molecules of the same MW
Glomerular and Peritubular Capillary Beds
Blood supply is via 2 capillary beds formed from the efferent arteriole.
- Peritubular capillary bed - supplies to cortex. Intertwined around PCT/DCT - reabsorbs anything from the tubular fluid back into the blood via renal venules + exits kidney via hilus
- VASA RECTA
Main blood supply to LOH + only blood supply to the medulla.
Renal Clearance : (in the tubular fluid) how much of a substance is removed vs. how much is retained
Clearance of a substance = Ux x V / Px
Ux = urine concentration of substance
Px = plasma concentration of substance
V = urine flow rate
RC shows the extent to which a substance is filtered at the glomerulus and its subsequent movements.
Glucose will have renal clearance of 0 as it will be retained by the body.
Substances that are added after filtration such as drugs will have a high renal clearance.
Substances that reflect GFR are ones that are freely filtered through the nephron ie. no reabsorption/secretion (inulin or creatinine)
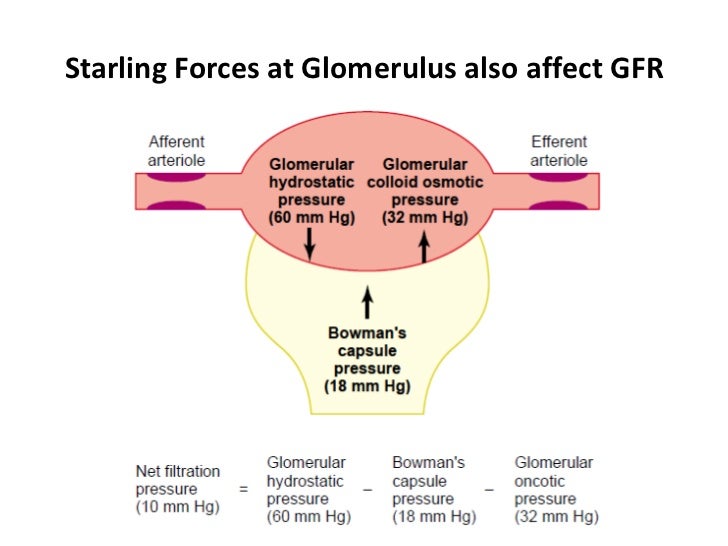
GFR also defined: KS (Pgc - Pt) - (πgc - πt). These forces are generated through the hydrostatic pressure of the blood through the heart.
2 forces that are forcing substances out of the blood into the tubular fluid.
Capillary hydrostatic: beating of the heart
Tubule colloid osmotic pressure: governed by presence of proteins. Proteins present in the tubule will draw substances out. BUT no proteins therefore negligible.
2 forces that are drawing substances back into the substance.
Capillary colloid osmotic pressure: presence of proteins in the capillary will draw substances back into the plasma. HIGH as proteins are retained.
Tubule hydrostatic - pressure from the tubule itself

There are minimum changes in Pgc and Pt as you move to the efferent arteriole. BUT changes seen in πgc .
V. thick with protein + cells as everything has been filtered out therefore no driving force for filtration therefore no filtration occurs.
Blood will have high colloid osmotic pressure and high haematocrit.
Regulation of Renal Blood Flow and GFR
GFR should be governed by BP (due to capillary hydrostatic pressure). But GFR remains constant despite BP. This is due to autoregulation.

Generally autoregulation occurs BUT it's more variable than thought. Some factors that can affect autoregulation include:

Renal Clearance : (in the tubular fluid) how much of a substance is removed vs. how much is retained
Clearance of a substance = Ux x V / Px
Ux = urine concentration of substance
Px = plasma concentration of substance
RC shows the extent to which a substance is filtered at the glomerulus and its subsequent movements.
Glucose will have renal clearance of 0 as it will be retained by the body.
Substances that are added after filtration such as drugs will have a high renal clearance.
Substances that reflect GFR are ones that are freely filtered through the nephron ie. no reabsorption/secretion (inulin or creatinine)
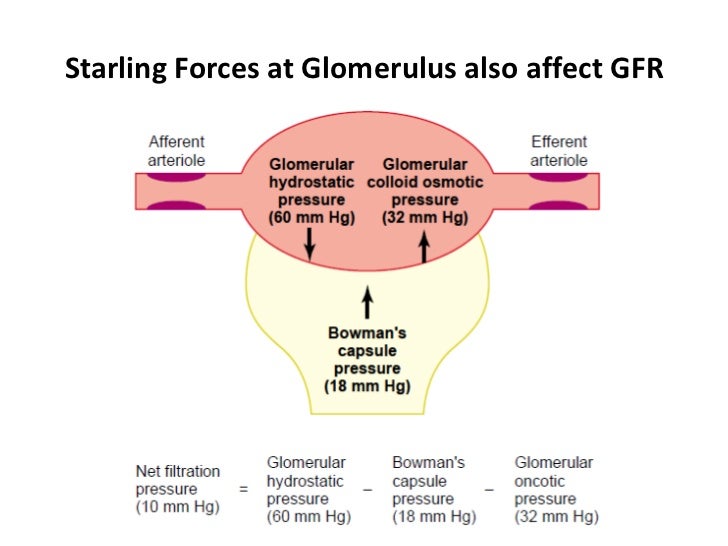
GFR also defined: KS (Pgc - Pt) - (πgc - πt). These forces are generated through the hydrostatic pressure of the blood through the heart.
2 forces that are forcing substances out of the blood into the tubular fluid.
Capillary hydrostatic: beating of the heart
Tubule colloid osmotic pressure: governed by presence of proteins. Proteins present in the tubule will draw substances out. BUT no proteins therefore negligible.
2 forces that are drawing substances back into the substance.
Capillary colloid osmotic pressure: presence of proteins in the capillary will draw substances back into the plasma. HIGH as proteins are retained.
Tubule hydrostatic - pressure from the tubule itself

There are minimum changes in Pgc and Pt as you move to the efferent arteriole. BUT changes seen in πgc .
V. thick with protein + cells as everything has been filtered out therefore no driving force for filtration therefore no filtration occurs.
Blood will have high colloid osmotic pressure and high haematocrit.
Regulation of Renal Blood Flow and GFR
GFR should be governed by BP (due to capillary hydrostatic pressure). But GFR remains constant despite BP. This is due to autoregulation.

Generally autoregulation occurs BUT it's more variable than thought. Some factors that can affect autoregulation include:
- Systemic BP
- Renal nervous input
- Endocrine influences
GFR can be measured when: rate of filtration = rate of excretion
Solute conc. in plasma, BC and Urine
Solute conc. in BC and plasma barely different except proteins
In urine, composition will change hugely:
- Range of Na+ dependent upon need
- Higher K+ due to K+ rich diets
- HCO3- mostly retained
- All of glucose is retained
Tubular Filtration
Everything that is filtered moves from BC - DCT - LOH. But if reabsorbed - it will go back into the arteriole.
Blood that leaves the efferent arteriole is v. thick - this is due too:
- High protein content - high haemtocrit as everything has already been filtered therefore the only thing that remains are large molecules that can't be filtered
- Low hydrostatic pressure as it has moved through the glomerulus
- High osmotic pressure - high conc. of proteins
As it is v. thick = slow movement through the peritubular capillaries and vasa recta so there is more time for substances to be reabsorbed.
Paracellular and Transcellular Pathways
Transcellular: through cells therefore crossing 2 membranes - apical membrane through intracellular fluid and basolateral membrane into blood
Paracellular: between cells, tight junctions into the lateral intracellular fluid
Both of these pathways occur in either direction eg. into tubule or blood
Anything against conc. gradient = TC (pumps)
PC = passive
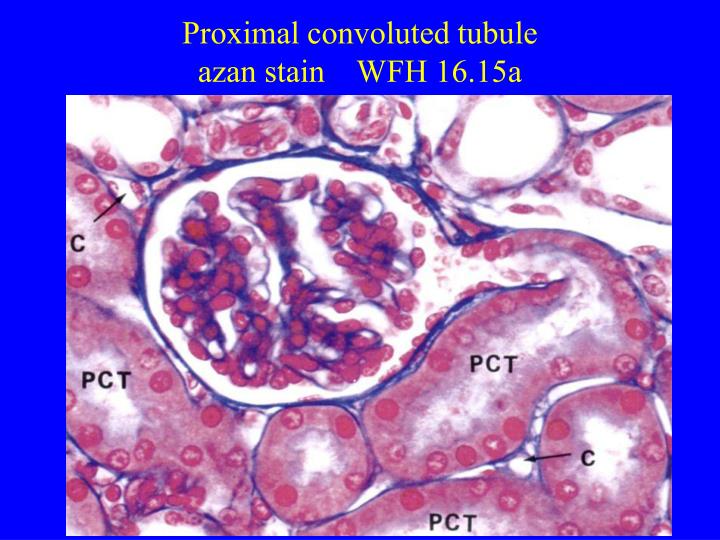
Proximal Convoluted Tubule
Reabsorbs 60-70% of glomerular filtrate therefore: brush border of microvilli + many mitochondria.
At the end of PCT - vol decreased but composition is almost identical to plasma.
Tubular Transport of Sodium
Most of Na+ is transported via 2nd active transport.
- Na+ moves down conc. gradient into tubular cells through Na+/H+ transporter by pumping H+ against conc. gradient into the lumen
- Low Na+ conc. inside the cell is maintained by Na+/K+ ATPase
- Na+ moves back down conc gradient into the cell and then pumped out at the basolateral membrane and diffuses back into blood in the peritubular capillaries back into the general circulation
Tubular Transport of Potassium and Calcium
Move paracellulary - between tight junctions down ionic conc. gradient
Some Ca2+ moves through cells
Ca2+ is pumped out into the interstitial fluid where substances end up before being moved into the blood via Starling's forces.
K+ pumped in via Na+/K+ ATPase = already high intracellular conc. therefore to retain more K+ it's pumped via ATPase pump. To remove K+, it will diffuse out via leak currents.
Tubular Transport of Glucose and Amino Acids
Occurs via 2nd active transport
- Na+ moves down conc. gradient + takes glucose with it (against conc. gradient) into the cell
- Moves into cells via specialised pumps (2nd AT)
- Removed from cells by faciliated diffusion across the basolateral membrane into the interstitum
If pumps are fully saturated ie. diabetes not all glucose is reabsorbed and is found in the urine. Known as transport maximum.
Tubular Transport of H2O: Water moves down its osmotic gradient - transcellular or paracellular
Tubular Transport of Bicarbonate and Hydrogen
Bicarbonate needs to be retained as it's a buffer. Needs to be reabsorbed but there are no bicarbonate transporters on the apical membrane.
- Bicarbonate combines with H+ to form carbonic acid
- In the presence of carbonic anhydrase, it breaks down to form H2O + CO2
- The products can easily move across the cells and reforms as bicarbonate in the blood
H+ is then removed in the DCT where it will continue to move around and facilitate this process.
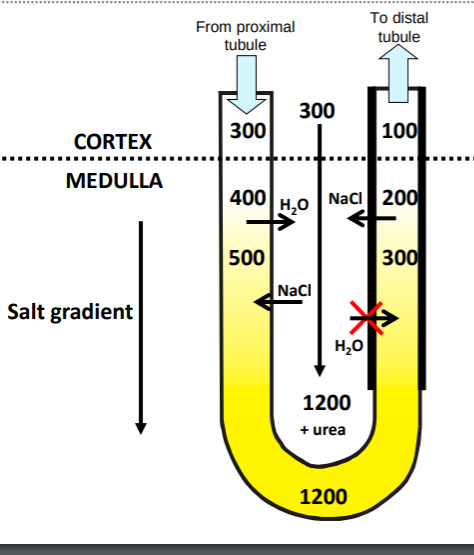
Countercurrent Multiplication in LOH
Tubular fluid is isosmotic and enters LOH.
It moves down the thin descending limb and H2O is drawn out as it gets more salty as you move deeper into the medulla.
Salt + H2O move freely - tubular fluid at the bottom of the LOH is the most conc.
Thick ascending limb is impermeable to H2O. But salt is pumped out via Na+/K+ chloride II transporter actively pumps salt into the interstitum allowing the osmotic gradient to be maintained.
The tubular fluid in the DCT is more dilute than when it first entered.
The LOH is subject to change in terms of length dependent upon water availability. The less H2O, the longer the loop the more likely you will absorb water and retain it as a steeper osmotic gradient is set up.

(Kangaroo Rat , lives in the desert)
Urine Concentrating Mechanism
Filtrate moves from DCT into collecting duct therefore affected by osmotic gradient. Therefore, if a person is dehydrated = aquaporins are opened to allow H2O to be drawn back out via the osmotic gradient that is set up.
If a person is sufficiently hydrated, gates will be closed to allow excess H2O to be excreted into the urine.
ADH affects the permeability of collecting duct.
DCT and Regulation of Potassium
DCT receives less than 20% glomerular filtrate.
DCT used in the regulation of K+ - it's reabsorbed in deficiency and secreted in hyperkalaemic states.
Aldosterone produced in the adrenal cortex and acts on distal nephron to
promote H+ and K
+
secretion via H+K
+ATPase
Hyperkalaemia
This is caused by the elevated K+ levels inactivating Na+ channels used to depolarised the heart whilst also opening up new K+ channels, leading to the heart becoming refractory.










Comments
Post a Comment